Neonatal hypogonadism due to rare testicular atrophy with congenital contralateral torsion: case report
Main Article Content
Abstract
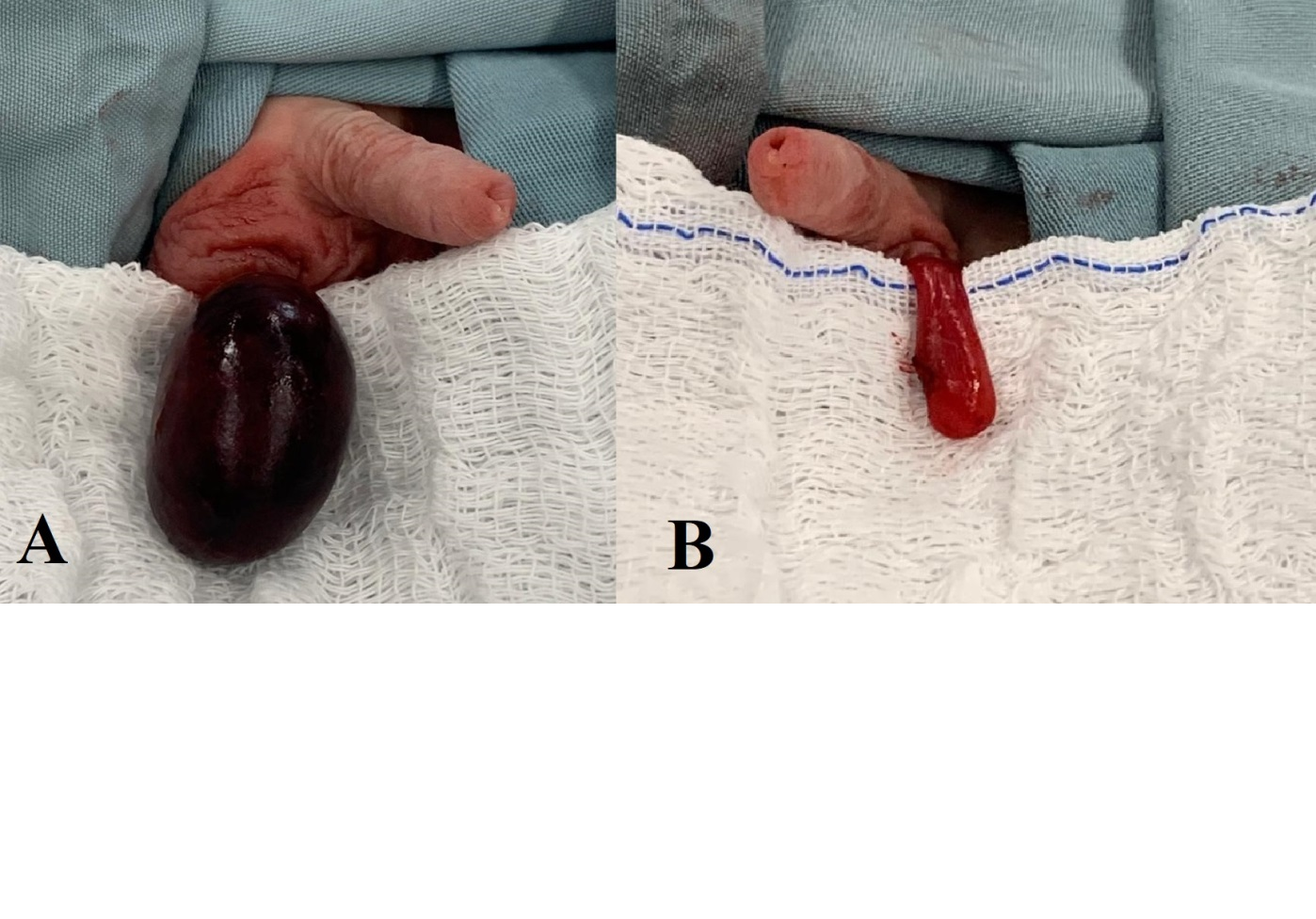
The process of sexual differentiation involves genetic, hormonal and anatomical factors, and there may be several disorders evident at birth. Congenital testicular torsion associated with atrophy contralateral gonad in phenotypically male newborns, without alteration in development of the internal and external genital organs, is a rare condition and little reported in the literature. Thereby, we sought to report and discuss the clinical case which the presence of both clinical conditions was diagnosed in the perinatal period. Hormonal production of testicular androgens is confirmed by the development of the male genital system, both internal and external. It isn’t possible to determine whether the atrophic testis was caused by extrinsic compression of the vascular bundle due to torsion of contralateral testis, or by testicular regression syndrome, in which there in involution of the organ in utero as part of presentation of gonadal dysgenesis. The twisted testicle may have been regression, without hormone production by it, or there was hormonal production of congenitally atrophied testicle and later regressed. Regardless of this fact, early diagnosis is the cornerstone of the clinical condition, since it will invariably evolve with hypergonadotropic hypogonadism, with need for multidisciplinary follow-up.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors retain the copyright of their articles and grant the journal the right of first publication under the Creative Commons Attribution (CC BY) license, which allows others to share and adapt the work with proper attribution.
References
Xu H, Zhang M, Zhang H, Alpadi K, Wang L, Li R, Qiao J. Clinical Applications of Serum Anti-Müllerian Hormone Measurements in Both Males and Females: An Update. Innovation (N Y). 2021 Feb 9;2(1):100091. doi: 10.1016/j.xinn.2021.100091.
Wilhelm D, Yang JX, Thomas P. Mammalian Sex Determination and Gonad Development. Curr Top Dev Biol. 2013;106:89-121. doi: 10.1016/B978-0-12-416021-7.00003-1.
Eggers S, Sadedin S, van den Bergen JA, Robevska G, Ohnesorg T, Hewitt J, et al. Disorders of sex development: insights from target gene sequencing of a large international patient cohort. Genome Biol. 2016;17(1):243. doi: 10.1186/s13059-016-1105-y.
Kim JH, Kang E, Heo SH, Kim GH, Jang JH, Cho EH, Lee BH, Yoo HW, Choi JH. Diagnostic yield of targeted gene panel sequencing to identify the genetic etiology of disorders of sex development. Mol Cell Endocrinol. 2017 Mar15;444:19-25.
Johannsen TH, Main KM, Ljubicic ML, Jensen TK, Andersen HR, Andersen MS, Petersen JH, Andersson AM, Juul A. Sex Differences in Reproductive Hormones During Mini-Puberty in Infants With Normal and Disordered Sex Development. J Clin Endocrinol Metab. 2018 Aug 1;103(8):3028-3037. doi: 10.1210/jc.2018-00482.
Castets S, Nguyen KA, Plaisant F, Prudon MB, Plotton I, Kassai B, Roche S, Ecochard R, Claris O, Nicolino M, Villanueva C, Gay CL. Reference values for the external genitalia of full-term and pre-term female neonates. Arch Dis Child Fetal Neonatal Ed. 2021 Jan;106(1):39-44.
de la Calle CM, Kim S, Baskin LS. Diagnosis and treatment of the intra-abdominal gonad in the pediatric population: Testes, ovaries, dysgenetic gonads, streaks, and ovotestes. J Pediatr Surg 2020; 55:2480. doi: 10.1016/j.jpedsurg.2020.02.014.
Loch Batista R, Inácio M, Prado Arnhold IJ, Gomes NL, Diniz Faria JA, Rodrigues de Moraes D, Frade Costa EM, Domenice S, Bilharinho Mendonça B. Psychosexual Aspects, Effects of Prenatal Androgen Exposure, and Gender Change in 46,XY Disorders of Sex Development. J Clin Endocrinol Metab. 2019 Apr 1;104(4):1160-1170. doi: 10.1210/jc.2018-01866.
Tanaka K, Ogasawara Y, Nikai K, Yamada S, Fujiwara K, Okazaki T. Acute scrotum and testicular torsion in children: a retrospective study in a single institution. J Pediatr Urol. 2020 Feb;16(1):55-60.
Feng S, Yang H, Lou Y, Ru W, Wang A, Liu W. Clinical Characteristics of Testicular Torsion and Identification of Predictors of Testicular Salvage in Children: A Retrospective Study in a Single Institution. Urol Int. 2020;104(11-12):878-883. doi: 10.1159/000506236.
Laher A, Ragavan S, Mehta P, Adam A. Testicular Torsion in the Emergency Room: A Review of Detection and Management Strategies. Open Access Emerg. Med. 2020;12:237–246. doi: 10.2147/OAEM.S236767.
Taghavi K, Dumble C, Hutson JM, Mushtaq I, Mirjalili SA. The bell-clapper deformity of the testis: The definitive pathological anatomy. J Pediatr Surg. 2021 Aug;56(8):1405-1410. doi: 10.1016/j.jpedsurg.2020.06.023.
Flück C, Nordenström A, Ahmed SF, Ali SR, Berra M, Hall J, Köhler B, Pasterski V, Robeva R, Schweizer K, Springer A, Westerveld P, Hiort O, Cools M. Standardised data collection for clinical follow-up and assessment of outcomes in differences of sex development (DSD): recommendations from the COST action DSDnet. Eur J Endocrinol. 2019 Nov;181(5):545-564. doi: 10.1530/EJE-19-0363.
Villar J, Cheikh Ismail L, Victora CG, Ohuma EO, Bertino E, Altman DG, Lambert A, Papageorghiou AT, Carvalho M, Jaffer YA, Gravett MG, Purwar M, Frederick IO, Noble AJ, Pang R, Barros FC, Chumlea C, Bhutta ZA, Kennedy SH; International Fetal and Newborn Growth Consortium for the 21st Century (INTERGROWTH-21st). International standards for newborn weight, length, and head circumference by gestational age and sex: the Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. Lancet. 2014 Sep 6;384(9946):857-68. doi: 10.1016/S0140-6736(14)60932-6.
Feldman KW, Smith DW. Fetal phallic growth and penile standards for newborn male infants. J Pediatr 1975; 86:395.
Pogorelić Z, Jukić M, Škrabić V, Mrklić I, Fridl Vidas V, Jurić I, Furlan D. Bilateral Simultaneous Testicular Torsion in a Newborn: Report of a Case. Acta Medica (Hradec Kralove). 2017;60(3):120-123.
Mellick LB, Sinex JE, Gibson RW, Mears K. A systematic review of testicle survival time after a torsion event. Pediatr Emerg Care. 2019;35:821–825. doi: 10.1097/PEC.0000000000001287
Nelson CP, Kurtz MP, Logvinenko T, Venna A, McNamara ER. Timing and outcomes of testicular torsion during the COVID-19 crisis. J Pediatr Urol. 2020;16:841.e1-e5.
Bay K, Main KM, Toppari J, Skakkebæk NE. Testicular descent: INSL3, testosterone, genes and the intrauterine milieu. Nat Rev Urol. 2011 Apr;8(4):187-96.
Koskenniemi JJ, Virtanen HE, Wohlfahrt-Veje C, Löyttyniemi E, Skakkebaek NE, Juul A, Andersson AM, Main KM, Toppari J. Postnatal Changes in Testicular Position Are Associated With IGF-I and Function of Sertoli and Leydig Cells. J Clin Endocrinol Metab. 2018 Apr 1;103(4):1429-1437. doi: 10.1210/jc.2017-01889.
Johannsen TH, Main KM, Ljubicic ML, Jensen TK, Andersen HR, Andersen MS, Petersen JH, Andersson AM, Juul A. Sex Differences in Reproductive Hormones During Mini-Puberty in Infants With Normal and Disordered Sex Development. J Clin Endocrinol Metab. 2018 Aug 1;103(8):3028-3037. doi: 10.1210/jc.2018-00482.
Harrison SM, Bush NC, Wang Y, Mucher ZR, Lorenzo AJ, Grimsby GM, Schlomer BJ, Büllesbach EE, Baker LA. Insulin-Like Peptide 3 (INSL3) Serum Concentration During Human Male Fetal Life. Front Endocrinol (Lausanne). 2019Sep4;10:596.
Sharma D, Sagar N, Khurana N. Testicular regression syndrome: A series of 22 cases at a tertiary care hospital. Trop J Pathol Microbiol. 2020;6(2):191-197. doi: 10.175111/jopm.2020.i02.12
Canales-Ramos NM, Burgos-Ortega NI, Grana-Santini AJ, Colon-Castellano JM, Gracia-Ramis A, Nieves-Rivera F, Alvarado M, Gonzalez-Rodriguez LA, Ramirez-Vick M. SUN-027 Testicular Regression Syndrome, an Underdiagnosed Cause of Hypergonadotropic Hypogonadism. J Endocr Soc. 2020 May 8;4(Suppl1):SUN-027.
Swee D, Quinton R. Current concepts surrounding neonatal hormone therapy for boys with congenital hypogonadotropic hypogonadism. Expert Review Endocrin Metabol. 2022;17(1):47-61.