Intraparenchymal Hemorrhage in a patient with Post-Traumatic Craniectomy and Severe Thrombocytopenia Due to Fatal Acute Dengue: A Case Report
Main Article Content
Abstract
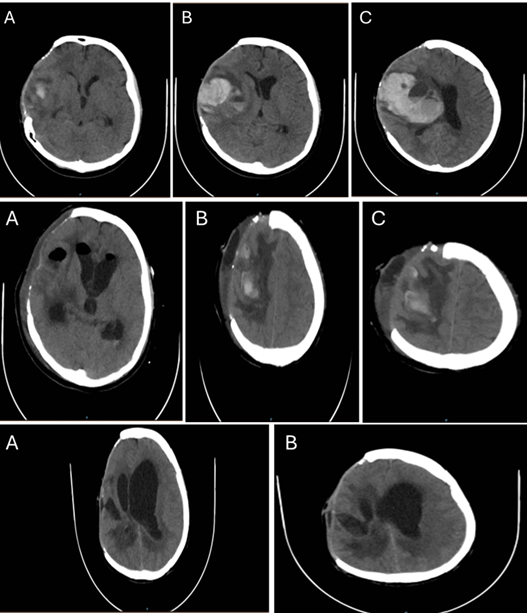
Intracranial complications in dengue fever are uncommon but have been increasingly reported in severe cases. Dengue fever is a mosquito-borne viral illness caused by the dengue virus, which usually presents mild symptoms such as fever, headache, and myalgia. In a minority of cases, the disease can progress to more severe forms characterized by plasma leakage, severe thrombocytopenia, and bleeding. Although neurological manifestations are not typical in dengue infections, factors such as severe thrombocytopenia and previous neurosurgical interventions may predispose patients to intracranial hemorrhagic events. This case report presents an 18-year-old female with a fatal intraparenchymal hemorrhage, occurring in the context of severe dengue and a history of prior post-traumatic craniectomy. This case illustrates how dengue-related thrombocytopenia and endothelial dysfunction can trigger catastrophic intracranial bleeding in areas of prior structural brain injury. Considering preexisting neurosurgical lesions as potential sites of secondary hemorrhage in dengue patients with severe thrombocytopenia.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors retain the copyright of their articles and grant the journal the right of first publication under the Creative Commons Attribution (CC BY) license, which allows others to share and adapt the work with proper attribution.
References
Kroeger A, Nathan M, Hombach J. Disease Watch: Dengue. Nat Rev Microbiol. 2004;2(5):360-1. doi:10.1038/nrmicro890.
Gubler DJ. Dengue and dengue hemorrhagic fever. Clin Microbiol Rev. 1998;11(3):480-96. doi:10.1128/CMR.11.3.480.
Castellanos J, Bello J, Velandia-Romero M. Dengue: aspectos virológicos, clínicos y epidemiológicos. Infectio. 2014;18(4):167-76. doi:10.1016/j.infect.2014.02.006.
Sil A, Biswas T, Samanta M, Konar MC, De AK, Chaudhuri J. Neurological manifestations in children with dengue fever: an Indian perspective. Trop Doct. 2017;47(2):145-9. doi:10.1177/0049475516679788.
Méndez A, González G. Dengue hemorrágico en niños: diez años de experiencia clínica. Biomedica. 2003;23(2):180-93. doi:10.7705/biomedica.v23i2.1210.
Domingues RB, Kuster GW, Onuki-Castro FL, Souza VA, Levi JE, Pannuti CS. Involvement of the central nervous system in patients with dengue virus infection. J Neurol Sci. 2008;267(1-2):36-40. doi:10.1016/j.jns.2007.09.040.
Carod-Artal FJ. Complicaciones neurológicas asociadas a la infección por el virus del dengue. Rev Neurol. 2019;69(3):113-22. doi:10.33588/rn.6903.2019140.
Cerejeido M, Shoshani L, Contreras RG. Molecular physiology and pathophysiology of tight junctions. I. Biogenesis of tight junctions and epithelial polarity. Am J Physiol Gastrointest Liver Physiol. 2000;279(3):G477-82. doi:10.1152/ajpgi.2000.279.3.G477.
Wasay M, Channa R, Jumani M, Shabbir G, Azeemuddin M, Zafar A. Encephalitis and myelitis associated with dengue viral infection: clinical and neuroimaging features. Clin Neurol Neurosurg. 2008;110(6):635-40. doi:10.1016/j.clineuro.2008.03.011.
Siahaan AMP, Tandean S, Ngan C, et al. A critical analysis of intracranial hemorrhage as a fatal complication of dengue fever. J Korean Neurosurg Soc. 2023;66(5):494-502. doi:10.3340/jkns.2022.0205.
Gubler DJ. Epidemic dengue/dengue hemorrhagic fever as a public health, social and economic problem in the 21st century. Trends Microbiol. 2002;10(2):100-3. doi:10.1016/S0966-842X(01)02288-0.
Srichaikul T, Nimmannitya S. Haematology in dengue and dengue haemorrhagic fever. Baillieres Clin Haematol. 2000;13(2):261-76. doi:10.1053/beha.2000.0073.
Carod-Artal FJ, Wichmann O, Farrar J, Gascón J. Neurological complications of dengue virus infection. Lancet Neurol. 2013;12(9):906-19. doi:10.1016/S1474-4422(13)70150-9.
Kumar R, Prakash O, Sharma BS. Intracranial hemorrhage in dengue fever: management and outcome: a series of 5 cases and review of literature. Surg Neurol. 2009;72(4):429-33. doi:10.1016/j.surneu.2009.01.021.
Jayasinghe NS, Thalagala E, Wattegama M, Thirumavalavan K. Dengue fever with diffuse cerebral hemorrhages, subdural hematoma and cranial diabetes insipidus. BMC Res Notes. 2016;9:265. doi:10.1186/s13104-016-2068-5.
García-Rivera EJ, Rigau-Pérez JG. Dengue severity in the elderly in Puerto Rico. Rev Panam Salud Publica. 2003;13(6):362-8.
Kutty RK, Balakrishnan S, Sivanandapanicker JL, Mundhe V, Chhabra K, Peethambaran A. Burden of dengue-related neu-rosurgical emergencies during an epidemic: a tertiary care experience. Asian J Neurosurg. 2019;14(1):211-8. doi:10.4103/ajns.AJNS_318_17.
Thadchanamoorthy V, Dayasiri K. Expanded dengue syndrome presenting with acute liver failure, acute kidney injury, pancreatic involvement, coagulopathy, and multiple intracranial hemorrhages in a young child. J Med Case Rep. 2022;16:148. doi:10.1186/s13256-022-03348-0.
Schreibman DL, Hong CM, Keledjian K, Ivanova S, Tsymbalyuk S, Gerzanich V, Simard JM. Mannitol and hypertonic saline reduce swelling and modulate inflammatory markers in a rat model of intracerebral hemorrhage. Neurocrit Care. 2018;29(2):253-63. doi:10.1007/s12028-018-0535-7.
Kung TFC, Kalisvaart ACJ, Suerte AC, Jickling GC, van Landeghem FKH, Colbourne F. No benefit of 3% hypertonic saline following experimental intracerebral hemorrhage. Neurotox Res. 2024;42(6):44. doi:10.1007/s12640-024-00722-2.
Mayung C, Thiodorus F, Yuliani D, Sumada IK, Jayanti KD. Spontaneous haemorrhagic stroke associated with expanded dengue syndrome: a case report. Int J Adv Med. 2023;10(4):289-93. doi:10.18203/2349-3933.ijam20230704.
Kaur R, Sharma A, Kumar S, et al. Expanded dengue syndrome presenting with multiple intracranial hemorrhages in a child: a case report. J Med Case Rep. 2022;16:148. doi:10.1186/s13256-022-03348-0.