Innovative Hemofiltration Approach to Protamine-Induced Shock After Cardiac Surgery in a Low-Resource Environment: A Case Report
Main Article Content
Abstract
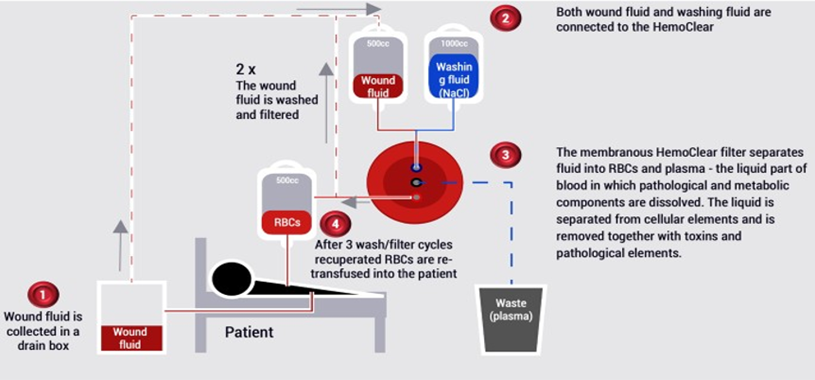
Protamine sulfate is routinely administered to reverse heparin anticoagulation following cardiopulmonary bypass (CPB). Although generally well tolerated, protamine may elicit severe hypersensitivity reactions, including anaphylaxis. Managing such complications is especially challenging in resource-limited settings where access to blood products and advanced supportive therapies is constrained. A 61-year-old man with multiple comorbidities underwent elective coronary artery bypass grafting (CABG). Following a 50 mg test dose of protamine sulfate after CPB, the patient developed profound hypotension and refractory shock unresponsive to vasopressors. Cardiac arrest ensued, prompting reheparinization and emergent reinstitution of CPB. Protamine was withheld after the second decannulation. Postoperatively, the patient experienced massive hemorrhage (~7 liters over 3 hours). Autologous blood was salvaged using a gravity-driven hemofiltration system (HemoClear®), with reinfusion of washed, platelet-rich red blood cells. Four units of FFP and albumin were administered. After stabilization, a reduced protamine dose (0.5 mg/kg) was safely administered for 2 hours postoperatively. The patient recovered without recurrence of adverse events. This case illustrates the importance of early recognition and tailored management of protamine-induced hypersensitivity reactions. In low-resource settings, gravity-driven hemofiltration may offer a feasible method of autologous blood salvage during critical hemorrhagic events.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors retain the copyright of their articles and grant the journal the right of first publication under the Creative Commons Attribution (CC BY) license, which allows others to share and adapt the work with proper attribution.
References
Kroeger A, Nathan M, Hombach J. Disease Watch: Dengue. Nat Rev Microbiol. 2004;2(5):360-1. doi:10.1038/nrmicro890.
Gubler DJ. Dengue and dengue hemorrhagic fever. Clin Microbiol Rev. 1998;11(3):480-96. doi:10.1128/CMR.11.3.480.
Castellanos J, Bello J, Velandia-Romero M. Dengue: aspectos virológicos, clínicos y epidemiológicos. Infectio. 2014;18(4):167-76. doi:10.1016/j.infect.2014.02.006.
Sil A, Biswas T, Samanta M, Konar MC, De AK, Chaudhuri J. Neurological manifestations in children with dengue fever: an Indian perspective. Trop Doct. 2017;47(2):145-9. doi:10.1177/0049475516679788.
Méndez A, González G. Dengue hemorrágico en niños: diez años de experiencia clínica. Biomedica. 2003;23(2):180-93. doi:10.7705/biomedica.v23i2.1210.
Domingues RB, Kuster GW, Onuki-Castro FL, Souza VA, Levi JE, Pannuti CS. Involvement of the central nervous system in patients with dengue virus infection. J Neurol Sci. 2008;267(1-2):36-40. doi:10.1016/j.jns.2007.09.040.
Carod-Artal FJ. Complicaciones neurológicas asociadas a la infección por el virus del dengue. Rev Neurol. 2019;69(3):113-22. doi:10.33588/rn.6903.2019140.
Cerejeido M, Shoshani L, Contreras RG. Molecular physiology and pathophysiology of tight junctions. I. Biogenesis of tight junctions and epithelial polarity. Am J Physiol Gastrointest Liver Physiol. 2000;279(3):G477-82. doi:10.1152/ajpgi.2000.279.3.G477.
Wasay M, Channa R, Jumani M, Shabbir G, Azeemuddin M, Zafar A. Encephalitis and myelitis associated with dengue viral infection: clinical and neuroimaging features. Clin Neurol Neurosurg. 2008;110(6):635-40. doi:10.1016/j.clineuro.2008.03.011.
Siahaan AMP, Tandean S, Ngan C, et al. A critical analysis of intracranial hemorrhage as a fatal complication of dengue fever. J Korean Neurosurg Soc. 2023;66(5):494-502. doi:10.3340/jkns.2022.0205.
Gubler DJ. Epidemic dengue/dengue hemorrhagic fever as a public health, social and economic problem in the 21st century. Trends Microbiol. 2002;10(2):100-3. doi:10.1016/S0966-842X(01)02288-0.
Srichaikul T, Nimmannitya S. Haematology in dengue and dengue haemorrhagic fever. Baillieres Clin Haematol. 2000;13(2):261-76. doi:10.1053/beha.2000.0073.
Carod-Artal FJ, Wichmann O, Farrar J, Gascón J. Neurological complications of dengue virus infection. Lancet Neurol. 2013;12(9):906-19. doi:10.1016/S1474-4422(13)70150-9.
Kumar R, Prakash O, Sharma BS. Intracranial hemorrhage in dengue fever: management and outcome: a series of 5 cases and review of literature. Surg Neurol. 2009;72(4):429-33. doi:10.1016/j.surneu.2009.01.021.
Jayasinghe NS, Thalagala E, Wattegama M, Thirumavalavan K. Dengue fever with diffuse cerebral hemorrhages, subdural hematoma and cranial diabetes insipidus. BMC Res Notes. 2016;9:265. doi:10.1186/s13104-016-2068-5.
García-Rivera EJ, Rigau-Pérez JG. Dengue severity in the elderly in Puerto Rico. Rev Panam Salud Publica. 2003;13(6):362-8.
Kutty RK, Balakrishnan S, Sivanandapanicker JL, Mundhe V, Chhabra K, Peethambaran A. Burden of dengue-related neu-rosurgical emergencies during an epidemic: a tertiary care experience. Asian J Neurosurg. 2019;14(1):211-8. doi:10.4103/ajns.AJNS_318_17.
Thadchanamoorthy V, Dayasiri K. Expanded dengue syndrome presenting with acute liver failure, acute kidney injury, pancreatic involvement, coagulopathy, and multiple intracranial hemorrhages in a young child. J Med Case Rep. 2022;16:148. doi:10.1186/s13256-022-03348-0.
Schreibman DL, Hong CM, Keledjian K, Ivanova S, Tsymbalyuk S, Gerzanich V, Simard JM. Mannitol and hypertonic saline reduce swelling and modulate inflammatory markers in a rat model of intracerebral hemorrhage. Neurocrit Care. 2018;29(2):253-63. doi:10.1007/s12028-018-0535-7.
Kung TFC, Kalisvaart ACJ, Suerte AC, Jickling GC, van Landeghem FKH, Colbourne F. No benefit of 3% hypertonic saline following experimental intracerebral hemorrhage. Neurotox Res. 2024;42(6):44. doi:10.1007/s12640-024-00722-2.
Mayung C, Thiodorus F, Yuliani D, Sumada IK, Jayanti KD. Spontaneous haemorrhagic stroke associated with expanded dengue syndrome: a case report. Int J Adv Med. 2023;10(4):289-93. doi:10.18203/2349-3933.ijam20230704.
Kaur R, Sharma A, Kumar S, et al. Expanded dengue syndrome presenting with multiple intracranial hemorrhages in a child: a case report. J Med Case Rep. 2022;16:148. doi:10.1186/s13256-022-03348-0.