Giant Cell Arteritis Presenting as Ischemic Stroke: A Case Report
Main Article Content
Abstract
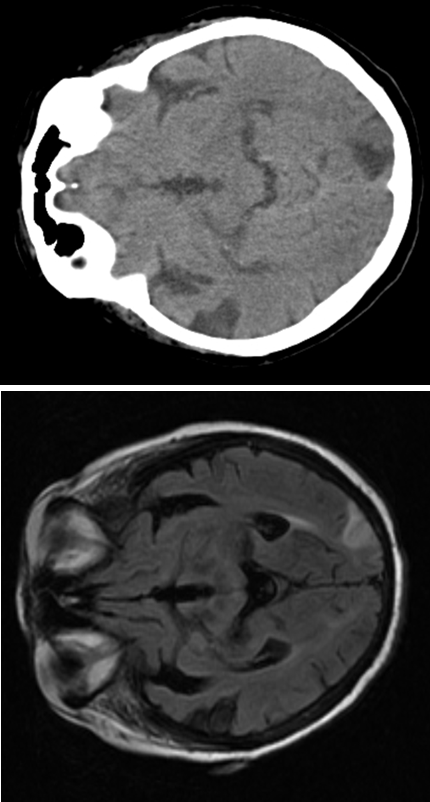
Giant cell arteritis (GCA) is the most common vasculitis over 50 years of age. GCA is an inflammatory condition affecting medium to large sized arteries. GCA is classified into a cranial form (c-GCA) and an extracranial/large vessel form (LV-GCA). Temporal artery doppler ultrasound (TADUS) has become the imaging modality of choice for GCA for rapid diagnosis. Glucocorticoids (GC) remain the primary treatment for GCA. We report the case of a 79-year woman with temporal headache, right hemiparesis and hypoesthesia. She had normocytic normochromic anemia, elevated c reactive protein (CRP) and erythrocyte sedimentation rate (ESR). Brain resonance (BR) revealed bihemispheric infarction. She was diagnosed with left sensorimotor lacunar cerebrovascular accident. TADUS revealed hypoechoic halo in the temporal arteries. c-GCA was newly diagnosed as the aetiology of stroke and treated with GC with resolution of symptoms. Ischaemic stroke is a rare complication in GCA and is a life-threatening condition. This case stands out for the importance of GC as an effective therapy in GCA with symptomatic intracranial involvement, improving their prognosis. In daily practice the early diagnosis of GCA can be challenging.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors retain the copyright of their articles and grant the journal the right of first publication under the Creative Commons Attribution (CC BY) license, which allows others to share and adapt the work with proper attribution.
References
Orfão A, Saca C, Alexandre O, Oliveira AM, Fernandes Serôdio J, Barreira J, et al. Giant cell arteritis presenting as multiple ischaemic strokes: a successful case of endovascular treatment. Eur J Case Rep Intern Med. 2024;11:004296.
van Nieuwland M, Boumans D, Plas G, Vijlbrief O, Alves C. A tale of diagnostic delay with detrimental consequences: illustrating the challenging nature of diagnosing giant cell arteritis. Eur J Case Rep Intern Med. 2021;8:2562. doi:10.12890/2021_002562.
Before symptomatic internal carotid artery stenoses can be attributed to giant cell arteritis, other causes must be ruled out. Eur J Case Rep Intern Med. 2024;11:4611. doi:10.12890/2024_004611.
Delaval L, Daumas A, Samson M, Ebbo M, Boysson H, Liozon E, et al. Large vessel vasculitis diagnosed between 50 and 60 years: case-control study based on 183 cases and 183 controls aged over 60 years. Autoimmun Rev. 2019;18(7):714-20.
Koster MJ, Warrington KJ. Classification of large vessel vasculitis: can we separate giant cell arteritis from Takayasu arteritis? Presse Med. 2017;46(3):e105-13.
Ponte C, Grayson PC, Suppiah R, Robson JC, Gribbons KB, et al. Classification criteria for large vessel vasculitis. Rheuma-tology (Oxford). 2019;58(5):736-45.
Dejaco C, Ramiro S, Duftner C, Besson FL, Bley TA, Blockmans D, et al. EULAR recommendations for the use of imaging in large vessel vasculitis in clinical practice. Ann Rheum Dis. 2018;77(5):636-43.
Schäfer VS, Juche A, Ramiro S, Krause A, Schmidt WA. Ultrasound cut-off values for intima-media thickness of temporal, facial and axillary arteries in giant cell arteritis. Rheumatology (Oxford). 2017;56(9):1479-83.
Luqmani R, Lee E, Singh S, Gillett M, Schmidt WA, Bradburn M, et al. The role of ultrasound compared to biopsy of temporal arteries in the diagnosis and treatment of giant cell arteritis (TABUL): a diagnostic accuracy and cost-effectiveness study. Health Technol Assess. 2016;20(90):1-238.
Prior JA, Ranjbar H, Belcher J, Mackie SL, Helliwell T, Liddle J, et al. Diagnostic delay for giant cell arteritis: a systematic review and meta-analysis. BMC Med. 2017;15(1):120.
Awisat A, Keret S, Silawy A, Kaly L, Rosner I, Rozenbaum M, et al. Giant cell arteritis: state of the art in diagnosis, monitoring, and treatment. Rambam Maimonides Med J. 2023;14(2):e0011. doi:10.5041/RMMJ.10496.
Yu E, Chang JR. Giant cell arteritis: updates and controversies. Front Ophthalmol. 2022;2:848861. doi:10.3389/fopht.2022.848861.
Farina N, Tomelleri A. Giant cell arteritis: update on clinical manifestations, diagnosis, and management. Eur J Intern Med. 2023;107:17-26. doi:10.1016/j.ejim.2022.10.025.
Paroli M, Caccavale R, Accapezzato D. Giant cell arteritis: advances in understanding pathogenesis and implications for clinical practice. Cells. 2024;13(3):267. doi:10.3390/cells13030267.
Bilton EJ, Mollan SP. Giant cell arteritis: reviewing the advancing diagnostics and management. Eye (Lond). 2023;37:2365-73. doi:10.1038/s41433-023-02693-6.