Eficácia da Troca Plasmática na Miastenia Gravis Após Longa COVID em um Contexto com Recursos Limitados: Relato de Caso
Conteúdo do artigo principal
Resumo
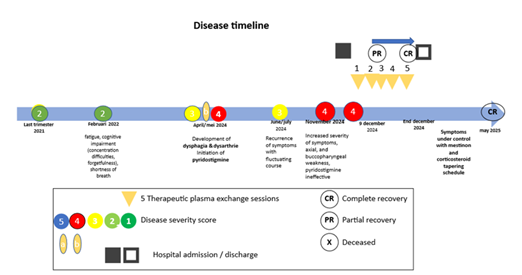
Este relato de caso descreve o desenvolvimento de miastenia gravis (MG) em um paciente do sexo masculino de 71 anos com COVID longa e detalha o manejo de uma exacerbação da MG. O paciente apresentou sintomas significativos, incluindo fadiga, comprometimento cognitivo, disfagia e disartria. Embora tenha sido observada melhora transitória após o tratamento com piridostigmina, a condição do paciente posteriormente se agravou, com fraqueza axial e bucofaríngea acentuada. O alívio dos sintomas foi finalmente alcançado por meio de plasmaférese utilizando um método de fluxo cruzado por gravidade de baixo volume. Este caso destaca o potencial impacto a longo prazo da COVID-19 em doenças autoimunes como a MG e reforça a necessidade de vigilância no manejo de complicações neurológicas pós-COVID.
Detalhes do artigo

Este trabalho está licenciado sob uma licença Creative Commons Attribution 4.0 International License.
Authors retain the copyright of their articles and grant the journal the right of first publication under the Creative Commons Attribution (CC BY) license, which allows others to share and adapt the work with proper attribution.
Referências
Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, et al. Post-acute COVID-19 syndrome. Nat Med. 2021 Apr;27(4):601-615. doi: 10.1038/s41591-021-01283-z.
Gilhus NE, Tzartos S. Bulbar symptoms and long-term prognosis in myasthenia gravis. Nat Rev Neurol. 2019 May;15(5):287-299. doi: 10.1038/s41582-019-0195-2.
Sanders DB, Wolfe GI, Benatar M, Evoli A, Gilhus NE, Illa I, et al. International consensus guidance for management of myasthenia gravis: Executive summary. Neurology. 2016 Jul 26;87(4):419-425. doi: 10.1212/WNL.0000000000002790.
Tugasworo D, Kurnianto A, Retnaningsih D, et al. The relationship between myasthenia gravis and COVID-19: A systematic review. Egypt J Neurol Psychiatr Neurosurg. 2022;58:83. doi: 10.1186/s41983-022-00516-3.
Bihariesingh-Sanchit R, Bansie R, Sam STA, Lieveld C, Simons A, Kromosoeto J, et al. Gravity-driven crossflow membrane filtration and mechanical centrifugation yield plasma with equivalent total and COVID-19-specific immunoglobulin content. World J Adv Res Rev. 2024;21(2):1107-1115. doi: 10.30574/wjarr.2024.21.2.0527.
Khatri BO, Raval JS. When and how to use plasma exchange therapy for difficult-to-treat multiple sclerosis patients. Inte-chOpen [Internet]. 2025 May 7 [cited 2025 Jun 7]; Available from: https://www.intechopen.com/online-first/1216614. doi: 10.5772/intechopen.1010410.
Restivo DA, Mazzone ME, Marchese-Ragona R, Centonze D, Alesina A. Myasthenia gravis associated with SARS-CoV-2 infection: A case report and review of the literature. J Neurol. 2022 Jan;269(1):45-48. doi: 10.1007/s00415-021-10785-2.
Sriwastava S, Shrestha AK, Khalid SH, Tandon M, Kataria S, Daimee M, et al. New-onset myasthenia gravis after SARS-CoV-2 infection: Case report and literature review. BMJ Case Rep. 2021 Sep;14(9):e244146. doi: 10.1136/bcr-2021-244146.
Dalakas MC. Autoimmune neurological syndromes triggered by COVID-19: A systematic review. Nat Rev Neurol. 2021 Mar;17(3):143-154. doi: 10.1038/s41582-020-00444-9.
Jacob S, Kapadia R, Soule T, Luo H, Schellenberg KL, Douville RN, et al. Neuromuscular complications of SARS-CoV-2 and other viral infections. Front Neurol. 2022;13:914411. doi: 10.3389/fneur.2022.914411.
Bihariesingh-Sanchit R, Bansie R, Ramdhani N, Mangroo R, Bustamente D, Diaz E, et al. Reduced mortality among COVID-19 ICU patients after treatment with HemoClear convalescent plasma in Suriname. mBio. 2023 Mar;14(2):e03379-22. doi: 10.1128/mbio.03379-22.
Jiang X, et al. Myasthenia gravis exacerbation and myasthenic crisis associated with COVID-19: Case series and literature review. J Neurol. 2020. doi: 10.1007/s10072-021-05823-w.
Roca E, et al. The relationship between myasthenia gravis and COVID-19: A systematic review. Egypt J Neurol Psychiatr Neurosurg. 2021. doi: 10.1186/s41983-022-00516-3.